Blog
OGM Champion Spotlight: Dr. Adam Smith, Cytogeneticist and Clinical Molecular Geneticist
Key Takeaways
- Reveal essential structural variant context: Using OGM to provide a complete view of SVs across the genome, finding pathogenic aberrations and resolving cryptic translocations.
- Eliminate guessing to solve complex clinical research challenges: Dealing with less ambiguity when interpreting cytogenomic results and using comprehensive and high-resolution profiles to better stratify sample risk.
- Build a global consensus: Dr. Smith founded an international consortium focused on hematological malignancies to build community and standardize OGM implementation.
- Streamline laboratory performance and maximize impact: How easy OGM workflow implementation empowered Dr. Smith’s lab and became their end-to-end research solution.
OGM Champion Spotlight: Dr. Adam Smith, Cytogeneticist and Clinical Molecular Geneticist
As a provider of genomic analysis solutions, Bionano enables researchers and clinicians from all over the globe to reveal answers to even the most complex and elusive challenges in medicine and biology. Complete with optical genome mapping (OGM), nucleic acid purification, testing services, and software, Bionano’s solutions are utilized across a wide array of applications including identifying structural variants in hematologic malignancies and solid tumors.
We sat down with Adam Smith, BSc, MSc, PhD, FCCMG, FACMG, erCLG, a dual-boarded clinical cytogeneticist and clinical molecular geneticist to discuss his utilization of OGM in hematological malignancy applications to solve complex research challenges, reveal essential structural variant context, build an international technique consensus, and streamline his laboratory’s performance to maximize their impact.
Q: Please tell us about your background and how you landed in the field of human genetic research.
I started my PhD at the Hospital for Sick Children in the University of Toronto, specifically looking at Beck Wiedemann Syndrome. I was interested in epigenetics and imprinting, and in how those molecular changes could be detected using different new technologies. I was accepted into a fellowship there where I was trained in clinical cytogenetics. After that I went to the BC Cancer Agency in British Columbia, and that was really where I was exposed to cancer and the very interesting genetic changes that we see in the disease. I then did a fellowship training program at the University Health Network in clinical molecular genetics, making me a dual-boarded clinical cytogenetic and molecular diagnostic lab director.
Legacy workflows vs OGM
Q: What techniques are available in your toolbox as a cytogeneticist?
We must talk about the elephant in the room when it comes to cytogenetics, and that’s the G-banded karyotype (KT). This is nearly a half a century old technique that’s been really quintessential. It allows us to see the genome in every individual cell so it’s a really important and powerful technique. As we work and look at different samples to try to figure out what’s going on genomically, the karyotype gives us a good view. But it suffers from serious limitations in that it’s unable to get down to the resolution we need to make important discoveries about the gene partners in unknown rearrangements. So, we’ve had a lot of ancillary techniques that have popped into the cytogeneticist’s toolbox over the years like fluorescence in situ hybridization (FISH) and chromosomal microarray (CMA) which have been very important. However, we’ve seen in certain cases where without the structural context, the interpretation of what a particular copy number change means can be very different. And this is where we’ve started to use optical genome mapping to get that structural context and see how interesting it’s been to bring all of this information together in a way and at a level of resolution that we haven’t been able to see before.
Q: Why is visualization of structural variants so critical, and why do you think that microarray technology has not become the standard of care for cancer?
Much of what’s important in hematological malignancies are the structural variants. If you look at the classification systems that we have for most of the different hematological malignancies, while there are copy number changes that are important, there are a lot of structural variants that are important to define. You have canonical changes like the translocation between chromosomes 9 and 22, known as the BCR-ABL1 rearrangement, that is diagnostic for chronic myeloid leukemia. And in acute myeloid leukemia, with the new WHO classification, an ever-growing list of defined genetic types of leukemia that are defined by their translocations. So, their detection is of paramount importance. And unfortunately, with microarray technology, we’re just not able to see them and the structural context in which these changes are happening.
Taking the guess work out of today’s complex research challenges
Q: As a clinical researcher, how many times do you get stuck with break-apart FISH probes and how much follow up testing is needed, especially in these cancer cases?
Every clinical research case we look at is a mystery. And it’s really important for biology that we understand the ramifications of these different rearrangements and how they affect outcomes for patients in the longer term. But what often happens is that when we get the results from our KT, we ask ourselves, “can it be this? Or maybe it’s that?” … And then we end up stacking up an infinite number of FISH probes, and still might not be able to resolve the case. So, we end up in a situation where we can’t really do anything more for the patient or research sample, and it’s frustrating.
We can make guesses, but those guesses can be very wrong. We had a research sample come in and we thought it was a particular translocation based on the karyotype. Then we did optical genome mapping and it turned out to be another gene that was close by, which could potentially lead to a different prognosis, or different therapies in a clinical setting. These are the interesting things that we see…When we use optical genome mapping, we don’t have to have a huge repertoire of ancillary testing available. We have the one test that we need, and it gives us a much more objective answer right off the bat and more quickly than doing multiple sequential analysis methods to try to resolve an ambiguous or subjective result that we get from a conventional cytogenetic test.
Q: Many publications we read are about samples on the 400 to 550 band level, but we know very clearly sometimes there are 300 band level or less, with very low resolution. Could you tell us more about that challenge?
I think the harsh reality that we deal with is that while it’s possible in some cancer samples to get relatively good chromosome banding preparations that give us relatively high resolution, and this maybe gives you in around 10 megabases of resolution, which is a relatively reasonable amount, but realistically speaking, a lot of the samples we get are not at that level of resolution. They might only be 300 to 350 band resolution, and these are very short chromosomes. This is where subjectivity creeps in because we can’t really say with a lot of certainty where the break points are, what the rearrangement is, if it’s a little bit more complex than a standard two segment exchange. And that really impacts the kind of answers that we’re giving because we’re not being clear about what the rearrangement is, what the mechanism is, or what the partners are. When we describe these different arrangements in leukemia, we need to be very clear and precise about what’s going on. And that’s where OGM was really surprising to me immediately–given its precision and objectivity.
Discovery of OGM and global advocacy efforts
Q: How did you come to find out about optical genome mapping?
I collaborated on a project with a colleague from the Princess Margaret Cancer Center looking at acute myeloid leukemia samples with complex karyotypes and looking at whole genome sequencing and RNA sequencing. It was obvious there were things we were missing by karyotyping, so we knew that it had certain limitations. We often use things like FISH or RT-PCR or another ancillary technique to find these things, but as you develop more single assay tests in the laboratory and your menu of testing starts to balloon, it becomes an ever-growing complex management problem for the laboratory. In 2020, I watched a presentation about optical genome mapping at a conference and I said, “this technology is going to change the way we do cytogenetics.” I went to the head of our department, and we recognized that there were multiple constraints in the department, not only the reagents and menu of testing I mentioned, but workflow constraints involving staff and logistics. We needed to find a technology that could simplify the lab workflow and give us the resolution that we needed to solve a lot of parallel problems at the lab at once–and that’s where our journey began.
Q: You’ve started this amazing initiative, the International OGM Heme Malignancy Consortium, where you have 25 to 30 key opinion leaders, laboratory directors, and principal investigators across multiple countries trying to standardize the implementation of OGM across the globe. Can you talk a little bit about what was the impetus for you to lead this initiative?
When we started using optical genome mapping, we realized early on that we’d have to make a lot of decisions like how we will analyze, interpret, and standardize this workflow. And that is a big question. You look at other techniques that we use in the lab, like karyotyping, that are very, very old, with lots of well-developed rules and systems that we use, but still subjective. When microarray came in, it took time for international guidelines to be established. So, one of the things that I felt is that we needed to collaborate right away. We needed to reach out to other people that are using optical genome mapping to move technology forward, build the OGM community, and build a consensus.
Streamlined workflow implementation and its real-life impact
Q: Can you speak about the benefits of the OGM workflow that you’ve seen?
A lot of diseases that we look at have samples that don’t divide very well in cell culture or even karyotyping them is hard because of how complex the profiles can be. Being able to pick out what’s important from the karyotype is a very challenging job. So, in many cases, we’re reflexing to FISH assays or others to help us clarify those types of rearrangements. So, in multiple myeloma, it’s very challenging because plasma cells are usually not very plentiful in the bone marrow aspirate. So, we do this process where we magnetically enrich the plasma cells to get a higher concentration. And this gives us a little bit of a better answer, but we’re still very limited because we have a fixed number of probes to use. I’ll be looking at a myeloma sample and I can rule out three of the five primary translocations, but I can’t rule out the final two and that’s very frustrating. And doing all of this karyotyping puts a huge demand on the laboratory–special mitogens, special culture techniques, et cetera. And that’s really what we’re looking forward to, this potential with optical genome mapping to use a single technique as a karyotype replacement, that will give us high-resolution mapping of the key actionable rearrangements that are important in these diseases.
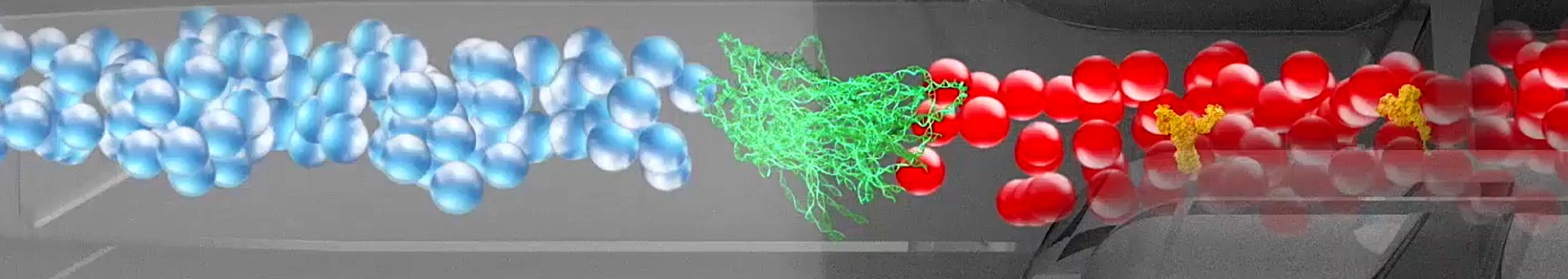
Optical genome mapping uses long DNA strands that have labels on them. It’s kind of a barcode and runs through the instrument through the nano channels to get imaged. Those images are bioinformatically processed, and they can be assembled against the reference genome to build a map. You’re looking where the labels are different from what they should be, except that the level of resolution is hundreds to thousands of times what it is for G-banded karyotyping. With optical genome mapping, we run the sample, we get the result, and that’s it. We’re done. We don’t need to do anything else. When we talk about the timeliness of getting that result completed and out, we can do that much more quickly in a single assay than with conventional techniques.
We bring in a new technology like optical genome mapping, and all of a sudden, we’re starting to see things we couldn’t see before. We can answer questions we weren’t able to answer before. There’s an immense satisfaction that comes from being able to really solve mysteries.
— Dr. Adam Smith
Ultimately knowing that solving those mysteries is helping somebody get treatment and figuring out what drives a particular cancer. That’s extremely rewarding.
Q: You are running your research cases and samples on a routine basis. What is the response from your laboratory technicians and other colleagues when you share this data?
The lab has been very excited about the technology right from the get-go. We brought the instrument in, and we started setting up our pilot project with our first year of samples and testing them compared to the conventional techniques. And we were surprised at how robust and fast we got going. We had field application scientists from Bionano come in and train us for a week. The next week we were running our own samples and, wow, analyzing our data. It was also very nice because we had everything we needed. We had kits to take it from sample to labeling to the instrument. We got the data and then we had the software to analyze it. We didn’t have to worry about other vendors or parties that were relying on custom bioinformatic pipelines. We had all of that in one solution. And when we started to share our results in much higher resolution, everyone was really, really excited about the prospects for a high resolution cytogenomic future.
With Bionano’s optical genome mapping we have an end-to-end solution. We have a software package that allows us to do analysis, and it’s the same software package that our colleagues are using in Europe or Australia or Japan when using optical genome mapping. We’ve been able to work collectively on a set of approaches that standardize the approach to interpretation analysis on the same software. And that has uniformly shown across multiple studies that there is a very high concordance between optical genome mapping results and their conventional counterparts.
After seeing the first sort of six months of data, we realized what a transformative potential optical genome mapping had for what we were doing day to day in the laboratory.